Part 1: The Pathway for Medicare Advantage Plans to Reach 5 Stars
During the COVID pandemic, CMS gave Medicare Advantage Plans an amnesty period, relaxing some of its stringency around Star measures. During that period, a record number of health plans achieved 4-star and above rankings. Those rankings led to billions of dollars in the form of rebates and quality bonus payments being paid to those plans. In 2023, CMS began applying increasingly stringent performance thresholds across many measures. The new thresholds resulted in a decline in the overall national Star Ratings for the second year in a row. In 2024, CMS implemented more new rules that create an even more difficult path for plans to achieve a 4-star rating or above.
CMS’ fundamental shift in its Stars reward framework, along with its ongoing need to drive cost containment, could result in the continued decline in Star Ratings for MA plans that fail to understand the implications of these changes and take action now.
This new three-part blog series explains what’s new, and how to address the changes effectively to improve outcomes and maintain or elevate your STAR Ratings in the new measurement year.
Understanding the Shift to the New Health Equity Index Reward
Already underway with the 2024 measurement period, CMS has implemented health equity as a core pillar of its goals. CMS replaced the current Reward Factor with the new Health Equity Index (HEI) reward in a major shift to link the Star Ratings to the highest risk populations among their overall membership. In previous contract years, health plans could receive an increase in their overall Star Ratings through the reward factor based on the quality performance of their entire membership. However, the HEI reward is now focused on solely on Dual-Eligible (DE), Low-Income Subsidized (LIS), and disabled membership.
Health plans that have relied on the current reward factor to reach a 4 Star Rating in the past need to pay close attention. Many of these plans have traditionally struggled with the hard-to-reach LIS/DE population. To remain viable, health plans must define new approaches to reach DE, LIS and disabled members, and invest in scalable, data-driven technology to support continual improvement in Star ratings.
Looking Deeper at DE, LIS and Disabled beneficiaries
CMS has defined DE, LIS, and disabled beneficiaries as those with Social Risk Factors (SRFs) and is pushing MA plans to provide service levels and drive quality performance for these members that is equal to or better than what is seen in traditional beneficiaries. The findings from a recent ActualMeds’ survey of 200 LIS/DE individuals make it clear why this population can be more challenging to reach for important measures like the triple weighted medication adherence.
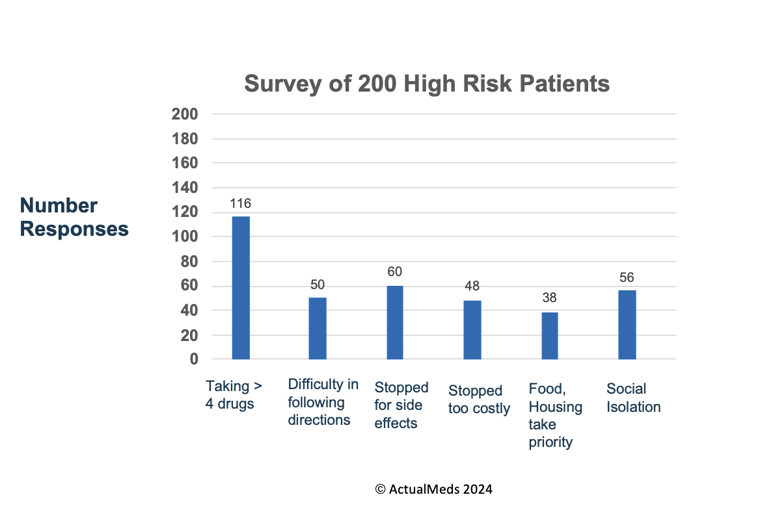
As part of an informal survey conducted by ActualMeds of 200 patients who were targeted based on DE/LIS and Disabled status, the following SRFs were reported by the respondents.

These SRFs, among others, can greatly affect adherence:
- 58% of respondents take more than 4 medications on a regular basis. Multiple chronic conditions and complex medication regimens are a hallmark of these high-risk populations and often lead to additional risks to adherence:
- 25% say that it is often or sometimes difficult to take medications as prescribed.
- 30% reported that they have stopped taking medications due to the side effects.
Economic factors also greatly impact these patients’ ability to access their medications in the first place:
- 24% said that they have stopped taking a medication because it was too costly.
- 19% have often or sometimes had to choose between buying prescriptions or paying for important things like food or a place to live.
- 28% reported feelings of loneliness or social isolation because these patients often are not surrounded by caregivers who can assist them with activities of daily living, including how and when to take their medications.
Addressing Social Risk Factors to Improve Health Equity at Scale
Developing a targeted strategy for the LIS and DE population matters because their needs are much more complex and less simple to resolve. Rather than just needing help with a refill or struggling to pay for a single medication, hard-to-reach LIS and DE members often need more guidance and support as their clinical risk profiles typically include multiple chronic conditions. Disabled patients have additional challenges that will be discussed in our next blog in this series.
In addition to compounding clinical factors, adherence to medication regimens for LIS and DE members can be impacted by other SRF barriers like access to transportation, or language barriers. . The new HEI reward factor now in place by CMS requires plans to have a deep understanding of how to structure programs for members with SRF’s. Simply sending more automated messages or placing more automated outbound calls will not resolve these barriers to adherence.
Improving Health Equity by Improving Medication Adherence
The HEI reward does offer an opportunity to health plans that have struggled in the past to reach a 4 Star rating. To take advantage of this reward, health plans need to focus more attention on the triple weighted adherence measures. These measures not only have a major influence on the overall STAR ratings for a health plan, but good medication adherence has been shown to reduce hospital admissions and readmissions for chronic diseases.
Having a scalable, human interaction increases medication adherence measures for even the most challenging, highest risk members. Relying on old methods to improve medication adherence is no longer an option. Health plans need to adapt and move forward, by leveraging tech-enabled services that use automated, data-driven processes to increase the probability of engagement. Using technology to identify the highest-risk beneficiaries reduces the need for manual, labor intensive activities allowing the pharmacy team to engage with more members, more effectively, and in concert with their overall care.
Finding the Right Partner to Manage Adherence Within the New CMS Health Equity Framework
- Among MA members for which ActualMeds’ provides end-to-end Stars Adherence Management, approximately 2/3 are LIS/DE and over 1/3 are Disabled status
- 71% LIS
- 62% Dual Eligible
- 37% Disability
For these members, we achieve an average of 4 Stars or higher consistently. ActualMeds technology streamlines workflows to enable our pharmacists to work to the top of their license to manage high risk patients; and for care coordinators to devote all of the time needed to connect patients with their providers, payers, and pharmacies to resolve barriers to adherence and to improve outcomes.
To learn more about how to get started with a new Stars strategy that prioritizes medication adherence and health equity, please visit our Stars solution page.


